- 7 months ago
- 14Minutes
- 2819Words
- 738Views
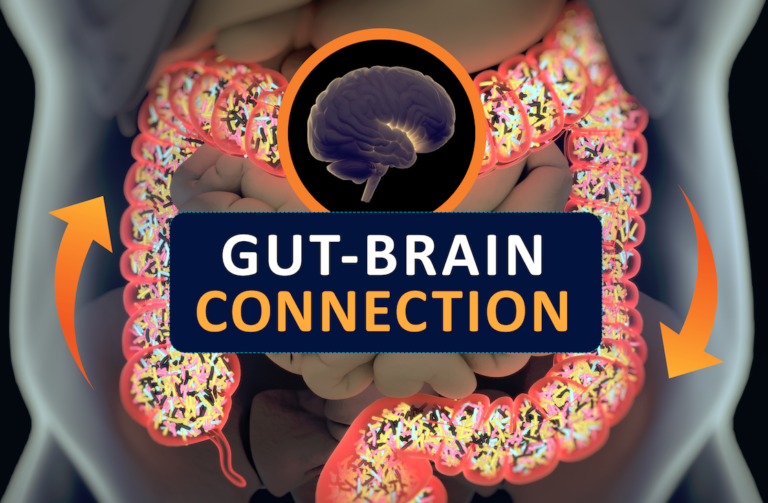
There has been a lot of talk about the gut-brain axis in recent years like it’s a new thing, but when you think about it we have always known about this gut-brain connection.
For example, we have adopted these common turns of phrase.
- I have a gut feeling about this
- My stomach is in knots
- Gut instinct
- Trust your feelings
- Let the force guide you (oops, that’s from Star Wars)
I think you get the idea. We’ve always known that our gut plays a role in our thought process and decision-making.
Today I’m going to share the 6 secrets to understanding your gut-brain health and what you can do to improve both.
(1) The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3997379/
(2) The Brain-Gut-Microbiome Axis. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047317/ (3) Mood, food, and obesity. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4150387/ (4) Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859128/ (5) Serotonergic Mechanisms Regulating the GI Tract: Experimental Evidence and Therapeutic Relevance. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5526216/ (6) Brain serotonin, carbohydrate-craving, obesity and depression. PUBMED https://www.ncbi.nlm.nih.gov/pubmed/8697046
On this page, we are going to explore 7 secrets to understanding the mechanisms within the gut-brain interface and how it affects our mental and physical health.
Hopefully, this can help you understand what practical things you can do to improve both gut and brain health, and overall happiness.
The 6 Secrets To Gut-Brain Health
Click the headings to skip to each.

Mental Health Statistics in Brief
Mental health issues are increasing worldwide, and it’s important to understand the scope. A review of 174 surveys found that about one in five adults (17.6%) experienced a common mental disorder in the past year, and one in three (29.2%) over their lifetime. (1)
In both high-income and low and middle-income countries, women are more likely to suffer from mood or anxiety disorders, while men are more prone to alcohol or substance use disorders. (1)
Standard pharmaceutical treatments for mental health issues focus on altering brain chemistry, but they can have severe side effects, including an increased risk of suicidal tendencies.
There’s a growing belief that if a person’s mental health problem is linked to emotional states and gut health, then simply using pharmaceuticals to mask the issue might not be effective. Over time, the unresolved gut feelings and emotions could become overwhelming.
This suggests a connection between mental health issues and digestive problems, including emotional or addictive eating habits. Therefore, understanding the link between gut health and brain chemistry is crucial for both physical and mental health.
The key interest lies in how gut health influences brain chemistry, a relationship that is complex and multifaceted.
Background to the Gut Brain Connection
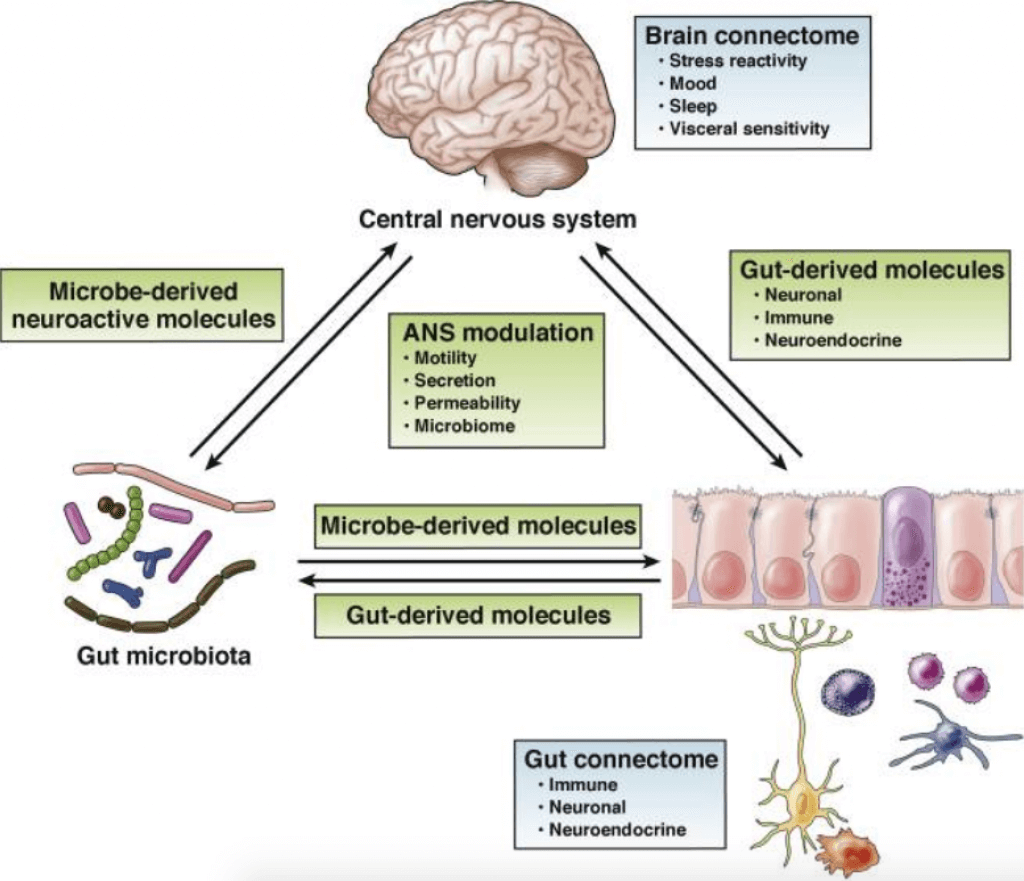
Over the last ten years, there has been a major shift in how we understand the connection between the brain and the gut. We now know that the gut microbiome (the collection of microorganisms living in the gut) and the brain communicate with each other in both directions.
This finding ties together the brain, gut, immune system, and the newly recognized gut-brain axis (GBA) into a comprehensive model. (2)
Research, including both laboratory and human studies, has revealed exciting possibilities for new treatments. These treatments are not just for gut-related issues, but also for a variety of mental and neurological conditions.
This includes Parkinson’s disease, autism spectrum disorders, anxiety, and depression, among others. (2)
Gut Health Issues that could affect Mental Health
Because the majority of the information highway (90%) between the gut and the brain is upwards from the gut, disturbances to gut health can affect our moods and mental health. Here are some common gut problems we can address to potentially improve mental health.
Acid Reflux
Candida overgrowth
Parasite infestation
Irritable Bowel Syndrome
Crohn’s Disease
Constipation
You can follow the links to read more on each condition, but right now, let’s talk about how our gut health actually has such a stronghold on our brain and mental state.
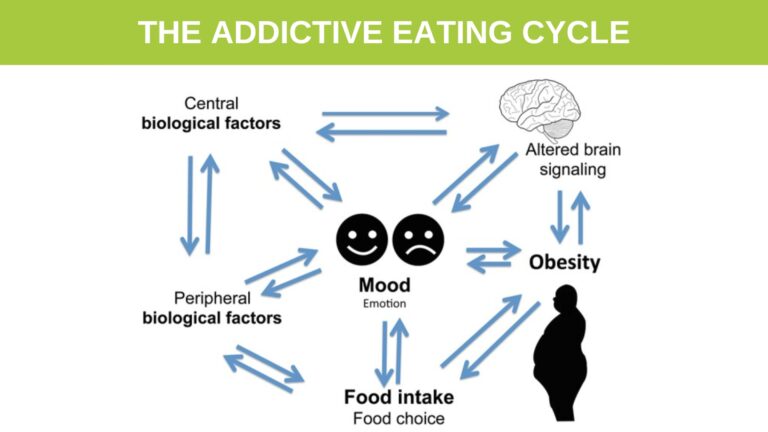
You can see the feedback mechanism between the brain, mood, food and obesity in the image below.
1. Where Imbalance Begins - Understanding Emotional Eating
First, let’s look at a couple of examples of how the gut-brain connection can start to affect us mentally, then we will look deeper into how this gut-brain axis (GBA) actually works on a biochemical level later on this page.
Altered moods such as stress, anxiety, frustration, etc. can lead to altered food choices, and intake, leading to overeating and obesity. This is often called ’emotional eating’. Research findings from human and animal studies support a two-way link between these three elements, mood, food, and obesity. (3)
Why do we reach for the wrong thing when we are going through a tough time emotionally?
It’s probably because we want a quick fix, and that’s what most of the high-calorie, sugar, chemical additives, and fat-rich foods can do. They give us a quick rush of energy to the brain which temporarily lifts our mood.
Drugs and alcohol are commonly abused for this very same reason.
The downside is, that the hormonal rush created by these stimulants does not last long, and in fact, the negative rebound effect is even more profound. We end up feeling worse for longer than we felt better, so we instinctively reach for the next hit. This is how emotional substance addiction begins.
We all know that stress and emotions affect our Gut, but just how profound are these effects?
- Mood disorders are often found in association with abnormal feeding behaviors. For example, depression and anxiety are often present with obesity. (3)
- Obese individuals are at increased risk of developing depression, and this risk is doubled in the presence of diabetes (3)
- Depressed mood is also associated with abdominal obesity and poor diet. (3)
- A link between obesity and depression has also been found in animal models of mood disorders. (3)
2. Gut Brain Physiology - Understanding The Vagus Nerve
Physiology of the Gut-Brain Axis
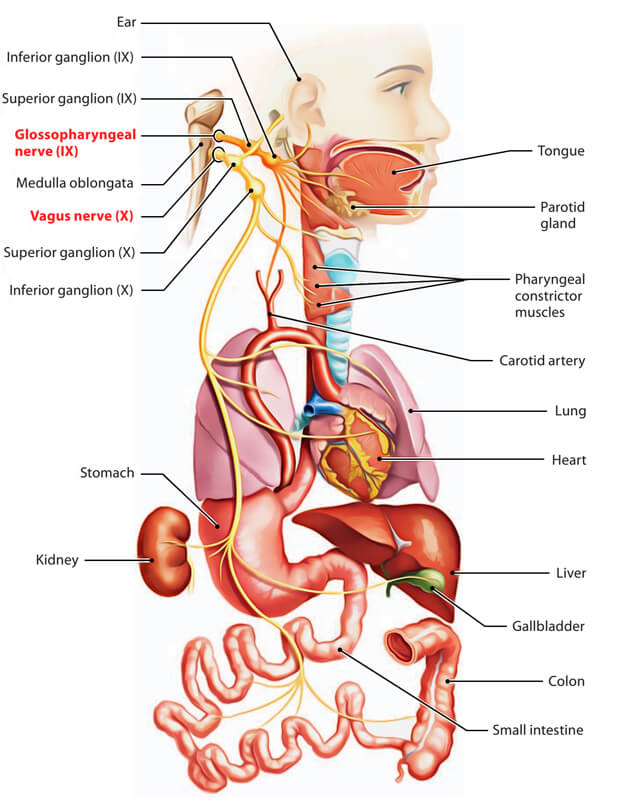
The vagus nerve is a key part of the parasympathetic nervous system, which controls many important functions in the body like mood, immune response, digestion, and heart rate. It connects the brain to the gastrointestinal tract and uses afferent fibers to send information about the internal organs back to the brain. (4)
There’s a two-way communication between the vagus nerve and the neurons in the gut. The primary method of this communication is through cholinergic activation, which happens via nicotinic receptors. This interaction between the gut neurons and the vagus nerve, which is part of the Central Nervous System (CNS), allows for information to flow in both directions.
Current research shows that the vagus nerve has receptors that can detect various signals from the gut, like peptides that regulate bodily functions, inflammatory molecules, components of our diet, and substances produced by gut bacteria. These signals are then transmitted to the brain. (2)
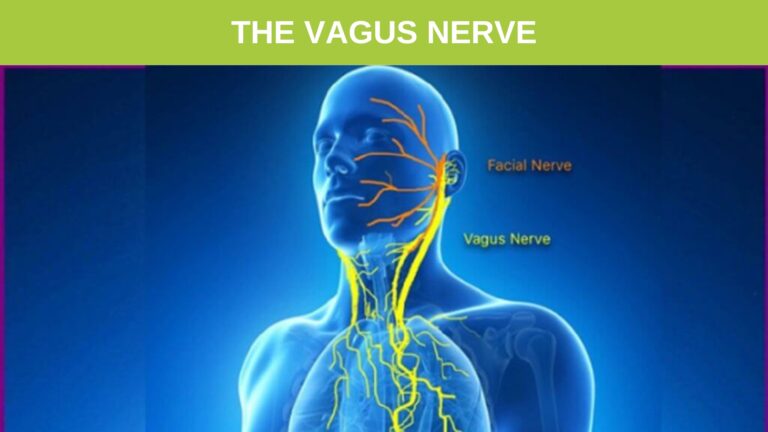
Early research suggests that adjusting the vagus nerve might help treat depression, post-traumatic stress disorder (PTSD), and inflammatory bowel disease. Treatments focusing on the vagus nerve can increase vagal tone (the nerve’s activity level) and reduce inflammation, both of which are key to mental resilience. (4)
Changing how the vagus nerve fibers in the gut work can also affect parts of the brain stem. These brain areas are important in managing major psychiatric conditions, including mood and anxiety disorders. (4)
There’s also evidence that gut bacteria can positively influence mood and anxiety. They do this partly by affecting the vagus nerve’s activity. Vagal tone, which is linked to how well we can handle stress, can be improved by practices like meditation and yoga. This improvement in vagal tone can help build resilience and lessen symptoms of mood and anxiety disorders. (4)
This diagram shows how the vagus nerve is connected to the digestive organs including the stomach, liver, and intestines.
3. How the gut Microbiome affects the Brain Hormonally
A key way that gut microbes communicate with the Central Nervous System (CNS) is through the hormonal system of the gut, known as the enteric endocrine system (EES). (2)
This is really worth taking a few minutes to understand, as it really explains why we feel so controlled by our gut and its emotions sometimes.
The Enteric Endocrine System
The enteric endocrine system (EES) cells are located among the regular cells lining the gut and are found throughout its entire length. These cells produce over 20 different types of signaling molecules. These molecules are released in response to chemical or physical triggers.
Once released, they can travel through the bloodstream to reach parts of the CNS that control eating behaviors, or they can work locally in the gut or liver to create brain signals. These EES cells have been found to have receptors that help regulate feelings of fullness and hunger. (2)
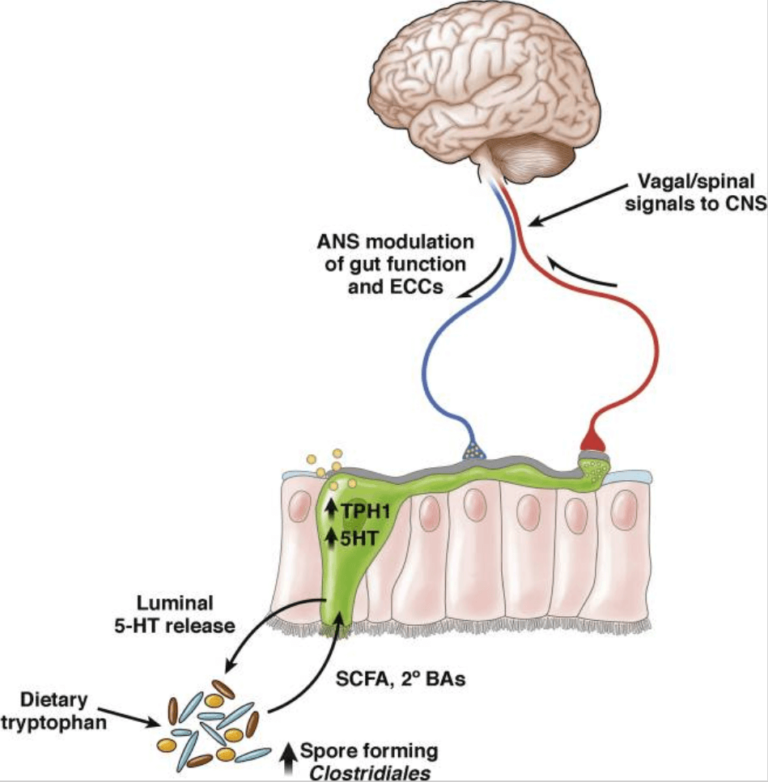
Serotonin (5-HT) Regulation
One of the most well-studied ways that microbes in the gut interact with the body involves a two-way relationship between these microbes, the enteric endocrine system (EES), and the central nervous system. A notable aspect of this interaction is the role of serotonin. The EES produces serotonin, with 95% of the body’s serotonin found in gut neurons and only 5% in the central nervous system and brain. (2)
The amino acid tryptophan (Trp) is crucial in the Gut-Brain-Axis (GBA) because it’s the building block for serotonin and other substances that play a role in the neuroendocrine communication within the GBA. Since humans can’t make tryptophan, it must come from our diet, primarily through proteins. Foods like milk and bananas are rich in tryptophan and are believed to help with relaxation and sleep. (2)
Gut bacteria affect how much tryptophan is available outside the central nervous system, which is important for making serotonin in the brain. Although the exact ways in which gut bacteria influence tryptophan levels are not fully understood, research suggests that these microbes may affect how tryptophan is broken down. One study even linked this interaction between tryptophan and gut bacteria to behavior. (2)
4. Foods and Herbs for Gut-Brain Health
This is a vast subject and we could have written much more, but in this instance, we have focused on the GBA and its mental health implications, especially in relation to the gut health.
Because I have seen over 120,000 people complete a Herbal Detox Program, which involves a diet of pure fruits and vegetables, I have seen thousands of my clients recover gut health.
The most surprising thing for many people is the sense of mental well-being, happiness, and peace they also experience after the detox.
The mechanics of the gut-brain axis give a clear explanation of why people feel so good during and after such an herbal health program.
Let me share some of the reasons food and herbs are so effective.
Herbs For The Brain
- Bacopa – Administration of BM appears to nourish rather than deplete neurons, an action compatible with 1400 years of Ayurvedic study.
- Ginkgo Biloba – Inhibits platelet aggregation (anti-PAF) to reduce blood viscosity, improves circulation.
- Gotu Kola – Studies have shown Gotu Kola to re-vitalize the brain and nervous system, increase attention span and concentration, and combat aging.
- St John’s wort – Helps to keep serotonin available in neuron synapses (spaces between nerve endings) of the brain. Take with professional guidance if using migraine drugs. St John’s wort protects the liver, nourishes, repairs, and calms the entire nervous system, and relieves pain.
- Bilberry – Blueberry intake has been shown to increase brain activity, memory, and learning and to decrease age-related cognitive decline. Cognitive performance in elderly adults improved after 12 wk of daily intake of blueberry.
- Turmeric – Strong anti-inflammatory, digestive, and liver support, blood thinning.
- Feverfew – Grow feverfew in the garden and chew on a few leaves when you experience a migraine aura. It is thought to work by inhibiting the generation and release of pro-inflammatory prostaglandins. Feverfew has also been shown to inhibit serotonin release from platelets, aiding blood vessel tone and constriction. This is a very bitter herb that promotes digestive secretions for improved food assimilation. Feverfew can also be taken prophylactically (as a preventative) – consume 2 to 3 leaves every day to reduce the frequency of migraines.
- Saffron – The active components in saffron protect neurons in the brain and increase the concentration of neurotransmitters in the synapses, thus enhancing cognitive function.
- Ginger – Another plant that improves blood circulation; inhibits thromboxane and other prostaglandins. Relieves inflammation, nausea, and vomiting.
Brett has formulated all of these herbs above into a wonderful liquid that you could take daily to help curb cravings and support Brain health.
Processed Foods Are Like Drugs
According to the research above, the overconsumption of processed foods high in sugar, additives, and fats causes a huge increase in serotonin release from the gut and brain. This is similar in effect to many addictive drugs, like alcohol and cigarettes, giving rise to food addiction.
These foods also interfere with a healthy gut microbiome and can trigger inflammatory bowel diseases, and the spin-off, like any drug addiction, can be depression, anxiety, and other forms of mental distress.
A vicious cycle begins, where addictive, emotional eating patterns lead to obesity, metabolic imbalances, and chronic mental health disturbances.
The Solution
To stabilize serotonin levels in the body and restore both gut and mental health a healthy diet needs to be followed. This will include high-fibre prebiotic foods, anti-inflammatory antioxidant-rich foods, and foods that supply low processed sugar and fat content, such as a variety of fresh fruits and vegetables.
Herbs can also play a major role in gut health by controlling yeast, negative bacteria, and parasites, contributing digestive enzymes, aromatic digestive oils, and wonderful flavours, which can curb cravings.
This is exactly what The Ultimate Herbal Health 14-day herbal detox program contains and explains why so many gut health and mental health issues appear to be addressed simultaneously.
You can read about the 24 Ultimate Detox herbs here
I hope you have found this article helpful and it has explained the gut-brain axis in a clear fashion.
More on Food Addiction
There are more than forty years worth of literature showing the effect of stress on the community structure of the gut microbiome. Exposure to social stressors for as little as 2 hours can change microbial community profiles and relative proportions. (2)
The autonomic nervous system, controlled by the hypothalamus in the brain, regulates gut functions including regional motility, secretion of gastric acid, mucus, bicarbonate, gut peptides, antimicrobial peptides, epithelial fluid maintenance, intestinal permeability, and mucosal immune response. These nervous-system-induced changes in gut physiology affect the microbial habitat, thereby modulating microbiota composition and activity. (2)
The key thing to note is that 95% of the body’s serotonin is stored in the intestinal neurons and this hormone is largely responsible for our feelings of emotional happiness and bliss. Because the signals “downward” from the brain to gut through vagus nerve fibers account for only 10–20% of all fibers and the “upward” from the intestinal wall to the brain accounting for 80–90% of all fibers, the gut is sending the majority of neural information upwards to the brain. (2)
Carbohydrate consumption increases serotonin release; while protein intake lacks this effect. This ability of neurons to couple neuronal signaling properties to food consumption is a link in the feedback mechanism that normally keeps carbohydrate and protein intakes more or less constant.
However, serotonin release is also involved in such functions as sleep onset, pain sensitivity, blood pressure regulation, and control of the mood. Hence many patients learn to overeat carbohydrates (particularly snack foods, like potato chips or pastries, which are rich in carbohydrates and fats) to make themselves feel better.
This tendency to use certain foods as though they were drugs is a frequent cause of weight gain, and can also be seen in patients who become fat when exposed to stress, or in women with premenstrual syndrome, or in patients with “winter depression,” or in people who are attempting to give up smoking.
It’s no wonder that this serotonin, feel-good, combination effect leaves us becoming addicted to foods, especially those junk/snack foods that trigger the release of serotonin sending pleasure signals to the brain and giving the consumer that quick-fix or high. (6)
The role of increased mucosal serotonin appears to be proinflammatory in its contribution to the process of intestinal inflammation. This evidence has led to a research focus on serotonin in intestinal inflammatory diseases. Mucosal serotonin reduction has been implicated in the modulation of several intestinal inflammatory diseases, including Crohn’s disease, ulcerative colitis, diverticulitis, and celiac disease. (5)
Animal models of intestinal inflammation have both confirmed the data from human studies and expanded our knowledge of the potential mechanisms underlying the role of mucosal serotonin in enteric inflammation and/or infection. (5)